Living with psoriasis can feel like an unending battle. The constant itching, discomfort, and visible skin changes can deeply affect your confidence, daily activities, and emotional well-being. If you or someone you know is navigating this chronic condition, it’s essential to remember that you are not alone. Psoriasis is a common, long-term autoimmune disease that affects millions of people worldwide, and understanding it is the most empowering step you can take.
This comprehensive guide is designed to be your go-to resource. It provides clear, medically accurate, and empathetic information to help you understand every aspect of psoriasis—from its fundamental causes and varied types to the wide range of available psoriasis treatment options. We’ll also cover practical psoriasis management strategies and debunk common myths. At Aakaar Medical Technologies Ltd, we are dedicated to providing innovative solutions that support individuals in their journey towards healthier skin and a better quality of life.
What is Psoriasis? A Chronic Autoimmune Condition Explained
Psoriasis is more than just a skin rash; it’s a systemic disease rooted in the immune system. In a healthy body, skin cells are produced deep in the skin and gradually rise to the surface, where they are shed every 28 to 30 days. This process is a natural cycle of cell renewal.
However, in people with psoriasis, the immune system mistakenly triggers an overactive response. This causes the production of new skin cells to accelerate dramatically, with cells maturing and rising to the surface in just 3 to 4 days. Since the body cannot shed these new cells quickly enough, they pile up on the surface of the skin. This rapid buildup leads to the characteristic thick, red, and inflamed patches covered with silvery-white scales, known as plaques.
While the primary symptoms appear on the skin, it is a chronic inflammatory disease that can affect other parts of the body, including the joints (psoriatic arthritis). Psoriasis is not contagious; you cannot transmit it through physical contact. Its chronic nature means that while symptoms can go into remission, the condition can flare up again at any time.
Causes of Psoriasis: The Genetic and Immune System Link
The exact causes of psoriasis are not fully understood, but research points to a complex interplay of genetic factors, immune system dysfunction, and environmental triggers.
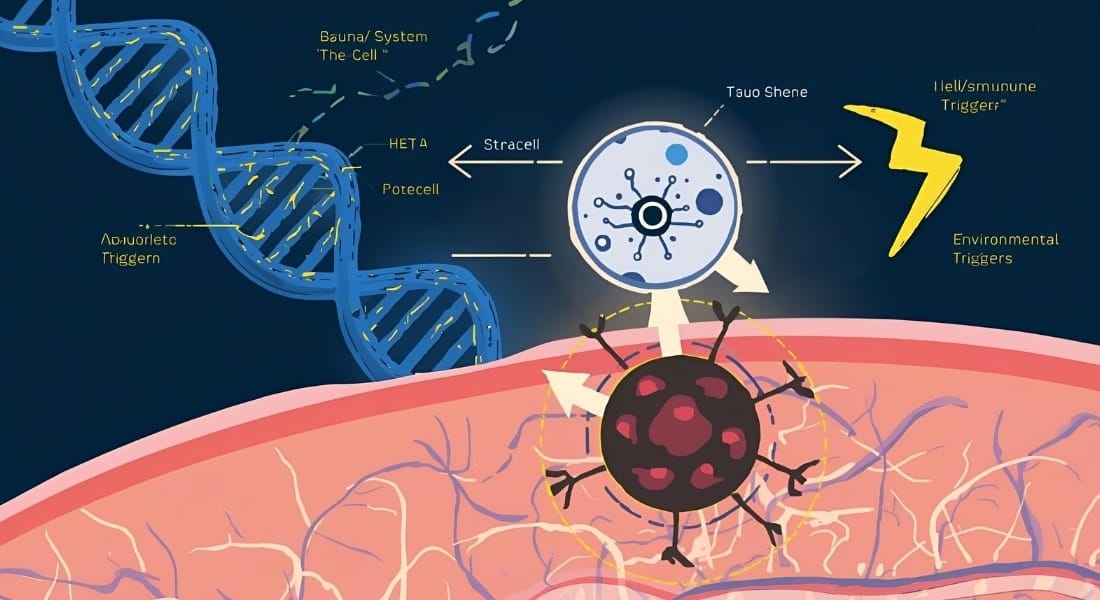
Genetic Factors
Psoriasis has a strong hereditary component. It often runs in families, and scientists have identified specific genes that are associated with an increased risk of developing the condition. This means that an individual may be genetically predisposed to psoriasis, but this does not guarantee they will develop it. A trigger is often needed to initiate the disease.
Immune System Dysfunction
Psoriasis is considered an autoimmune disease because the immune system plays a central role. T-cells, a type of white blood cell, are designed to protect the body from foreign invaders like bacteria and viruses. In psoriasis, these T-cells become overactive and mistakenly attack healthy skin cells. This attack triggers a chain reaction of inflammation and speeds up the production of new skin cells, leading to the formation of plaques. This is why many psoriasis treatment options focus on modulating or suppressing this immune response.
Environmental Triggers
Even with a genetic predisposition and an overactive immune system, psoriasis often needs an external trigger to appear for the first time or to cause an existing condition to flare up. Common triggers include:
- Stress: High levels of psychological stress are a well-documented trigger. Stress can make existing symptoms worse or cause a new flare.
- Infections: Bacterial infections like strep throat are a common trigger for a specific type of psoriasis called guttate psoriasis, especially in children and young adults.
- Skin Injury: A phenomenon known as the Koebner phenomenon means that a skin injury—such as a cut, scrape, bug bite, severe sunburn, or even a vaccination—can cause new psoriatic plaques to form at the site of the injury.
- Medications: Certain medications, including beta-blockers (for high blood pressure), lithium, and some anti-malarial drugs, can trigger or worsen psoriasis symptoms.
- Cold, Dry Weather: Cold weather and a lack of humidity can dry out the skin and trigger a flare-up.
Types of Psoriasis: Recognizing the Variations
Psoriasis is not a single condition; it has several distinct forms, each with unique signs and symptoms. Understanding the different types of psoriasis is a key part of getting an accurate diagnosis and a personalized treatment plan.
Plaque Psoriasis (Psoriasis Vulgaris)
This is the most common form, affecting about 80-90% of people with psoriasis.
- Appearance: Characterized by raised, red patches of skin, often with a silvery-white, scaly buildup on top. These patches can be itchy and painful and may crack or bleed.
- Common Locations: Most often found on the elbows, knees, lower back, and scalp.
Guttate Psoriasis
- Appearance: Appears as small, red, individual spots (resembling raindrops) scattered over the body, most commonly on the trunk, arms, and legs.
- Trigger: It is often triggered by a bacterial infection like strep throat and is more common in children and young adults.
Inverse Psoriasis (Flexural Psoriasis)
- Appearance: Develops in skin folds, such as in the armpits, groin, under the breasts, and around the genitals. The patches are smooth, red, and inflamed, typically lacking the scales seen in other types due to the moist environment of these areas.
- Challenges: Friction and sweating can make this type of psoriasis particularly uncomfortable and prone to fungal infections.
Pustular Psoriasis
- Appearance: Characterized by clearly defined, pus-filled bumps (pustules) surrounded by red, inflamed skin. The pus is not infectious; it is a build-up of white blood cells.
- Severity: Can be localized to a small area (e.g., the palms of the hands and soles of the feet) or, in a rare and serious form, spread across large areas of the body.
Erythrodermic Psoriasis
- Appearance: The rarest and most severe form of psoriasis, covering nearly the entire body with a fiery red, peeling rash.
- Danger: It can disrupt the body’s temperature regulation and fluid balance, leading to severe illness and requiring immediate medical attention.
Symptoms of Psoriasis: What to Look For
The psoriasis symptoms can vary in severity and appearance, but they often include a combination of the following:

- Red, inflamed patches of skin with thick, silvery-white scales
- Dry, cracked skin that may bleed or feel painful
- Itching, burning, or soreness around the affected areas
- Thickened, pitted, or ridged fingernails and toenails
- Swollen and stiff joints (in cases of psoriatic arthritis)
- Small scaling spots, particularly in children (guttate psoriasis)
If you notice any of these signs, especially if they are persistent or interfere with your quality of life, it’s important to consult a dermatologist.
Risk Factors & Triggers: Managing Your Condition
While you can’t change your genetics, understanding and managing the risk factors and triggers can help you control your psoriasis more effectively.
- Stress: Chronic stress is a significant trigger for many people with psoriasis.
- Smoking: Smoking not only increases the risk of developing psoriasis but also makes it more severe and harder to treat.
- Alcohol Consumption: Excessive alcohol intake can trigger flares and may negatively interact with certain medications.
- Cold Weather: Dry, cold climates tend to worsen psoriasis, while warm, sunny weather often provides relief.
- Certain Medications: As mentioned, be sure to discuss your condition with your doctor before starting new medications.
- Skin Injuries: Avoid scratching plaques and take care to protect your skin from cuts, scrapes, and bug bites.
Diagnosis: Getting an Accurate Assessment
An accurate diagnosis is the first step toward effective psoriasis management. A dermatologist can usually diagnose psoriasis through a simple clinical examination.
- Clinical Examination: Your doctor will examine your skin, scalp, and nails for the characteristic signs of psoriasis.
- Skin Biopsy: In some cases, to rule out other skin conditions like eczema or a fungal infection, your doctor may take a small skin sample (biopsy) to be examined under a microscope.
- Differentiating from other conditions: Psoriasis can look similar to other conditions, such as seborrheic dermatitis or ringworm. An experienced dermatologist can tell the difference.
Psoriasis Treatment Options: Finding Your Path to Relief
While there is no cure, a wide range of effective psoriasis treatment options can help manage symptoms, achieve clear skin, and improve your overall well-being. The best treatment plan is always personalized based on the type and severity of your condition, as well as your lifestyle and preferences.
1. Topical Treatments
These are often the first line of defense for mild to moderate psoriasis. They are applied directly to the skin to reduce inflammation and slow down cell growth.
- Corticosteroids: Reduce inflammation and are available in various strengths.
- Vitamin D Analogues: Regulate skin cell growth and are often combined with corticosteroids.
- Retinoids: Help to reduce inflammation and normalize cell turnover.
- Moisturizers: An essential part of any psoriasis care products routine, moisturizers help soothe dry, scaly skin and reduce itching.
2. Phototherapy (Light Therapy)
This treatment involves exposing the affected skin to a controlled dose of natural or artificial ultraviolet (UV) light. It works by slowing down the rapid growth of skin cells.
3. Systemic Treatments
For moderate to severe psoriasis that doesn’t respond to topical treatments or phototherapy, doctors may prescribe systemic medications, which work throughout the body.
- Oral Medications: Immunosuppressants like methotrexate and cyclosporine or newer targeted oral medicines.
- Injectable Medications: Biologics are a class of targeted therapies that block specific parts of the immune system responsible for psoriasis. They are a significant advancement in psoriasis treatment.
4. Ayurvedic/Alternative Approaches
In many cultures, including India, patients may explore traditional remedies to complement their medical treatment. While the scientific evidence for many of these is limited, some individuals find them helpful in managing symptoms.
We at Aakaar Medical Technologies Ltd are proud to offer the Tinefcon Range as an innovative, supportive approach to psoriasis management. Tinefcon is an oral formulation derived from a globally patented phytoactive ingredient. It works by targeting specific inflammatory pathways to help balance the immune response and reduce the severity of symptoms like redness, scaling, and itching. Unlike some conventional systemic treatments, Tinefcon is designed to be a safe, non-immunosuppressive option for long-term use. This makes it an ideal choice as a standalone treatment or as part of a comprehensive psoriasis care products regimen.
Lifestyle & Self-Care Tips for Psoriasis Patients
Managing your condition is a daily practice. Here are some simple but effective tips:

- Skincare Routine:
- Moisturize multiple times a day, especially after bathing, to keep skin hydrated and supple.
- Use lukewarm water instead of hot water in the shower or bath, and opt for gentle, fragrance-free soaps.
- Stress Management: Psoriasis and stress can create a vicious cycle. Practice mindfulness, meditation, yoga, or deep breathing to help calm your mind and body.
- Diet & Nutrition: While no single diet cures psoriasis, some patients find that reducing inflammatory foods (like red meat and processed foods) and increasing anti-inflammatory foods (like omega-3 fatty acids from fish, fruits, and vegetables) can help.
- Stay Hydrated: Drinking plenty of water is essential for overall skin health.
Myths vs Facts about Psoriasis: Separating Truth from Fiction
Misconceptions about psoriasis can lead to stigma and isolation. It’s important to know the facts.
- Myth: Psoriasis is contagious.
- Fact: Psoriasis is a non-communicable, autoimmune disease. You cannot catch it from someone or spread it through physical contact.
- Myth: Psoriasis is a result of poor hygiene.
- Fact: Psoriasis has nothing to do with cleanliness. It is an internal disorder of the immune system.
- Myth: Psoriasis can be cured.
- Fact: Currently, there is no cure for psoriasis. However, it is highly manageable with the right treatment and lifestyle choices, allowing for long periods of remission.
- Myth: Psoriasis only affects the skin.
- Fact: Psoriasis is a systemic disease. It can lead to other health conditions, most notably psoriatic arthritis, which affects the joints.
Living with Psoriasis: Patient Guidance and Support
Living with a chronic condition can be tough, but you can thrive.
- Coping Strategies: Find healthy ways to cope with the emotional toll. This could include talking to friends and family, joining a support group, or consulting a mental health professional.
- Support Groups: Connecting with other patients who truly understand your experience can reduce feelings of isolation and provide a valuable source of information and encouragement.
- Regular Doctor Visits: Stay in regular contact with your dermatologist. Regular check-ups are vital for monitoring your condition and adjusting your psoriasis treatment plan as needed.
When to See a Doctor
It’s important to know when to seek medical help for your psoriasis.
- Your symptoms are worsening or are not responding to over-the-counter remedies.
- You experience signs of psoriatic arthritis, such as joint pain, stiffness, or swelling.
- The psoriasis is affecting your daily activities, sleep, or emotional well-being.
- You are experiencing a flare that is widespread or covers a large area of your body.
Frequently Asked Questions
Q1: Is psoriasis curable?
A: No, psoriasis is a chronic condition and is not currently curable. However, with effective psoriasis treatment and management, many people can achieve long periods of remission where symptoms are minimal or absent.
Q2: Can psoriasis be confused with eczema?
A: Yes, psoriasis and eczema are often mistaken for each other because they both cause red, itchy rashes. However, psoriasis typically results in thicker, more well-defined plaques with silvery scales, whereas eczema rashes are often more patchy and intensely itchy. A dermatologist can make an accurate diagnosis.
Q3: Are there any natural remedies for psoriasis?
A: Many patients find that complementary approaches, such as stress management, dietary changes, and using natural moisturizers, can help manage their symptoms. However, it’s important to consult with your doctor before starting any new psoriasis care products or treatments to ensure they are safe and will not interfere with your existing regimen.
Q4: Can diet affect my psoriasis symptoms?
A: While there is no “psoriasis diet,” some people find that certain foods can trigger or worsen their symptoms due to inflammation. Adopting an anti-inflammatory diet rich in fruits, vegetables, and lean proteins may help, but this varies from person to person.
Q5: What is the best treatment for psoriasis?
A: The “best” psoriasis treatment is highly individual. It depends on the type and severity of your psoriasis, as well as your personal health and lifestyle. A dermatologist will work with you to create a personalized plan that may include topical creams, phototherapy, systemic medications, or a combination of approaches.
Conclusion: Partnering for a Brighter Future in Aesthetics

Psoriasis is a lifelong condition, but it is not one that has to control your life. By understanding the fundamentals of what is psoriasis and actively engaging in a personalized psoriasis management plan, you can take control and achieve a significant improvement in your skin and overall well-being. The evolution of aesthetic and medical science provides extraordinary opportunities for effective management and improved quality of life.
We at Aakaar Medical Technologies Ltd are committed to being a partner in this journey, providing advanced, scientifically backed solutions. We encourage you to explore our innovative Tinefcon Range as a supportive and effective option to help you on your path to healthier skin.

